Abstract
Background: Across the human lifespan, an age-related decline in immunocompetence and a concurrent increase in chronic inflammation are evident. The Philadelphia-negative myeloproliferative neoplasms (MPNs) represent a heterogeneous group of acquired hematopoietic stem cell diseases where chronic inflammation is essential for both the clonal evolution and development of comorbidities prior to and after diagnosis.
Neutrophilic heterogeneity is well described where neutrophils have the capability to inhibit T-lymphocytes and natural killer cells, potentially implying reduced immune competence, which may enhance the clonal progression and evolution of the malignant clone. Thus, the neutrophil-to-lymphocyte ratio (NLR) is a simple biomarker index that both encapsulates chronic inflammation and reduced immune competence. Increased NLR is associated with several inflammatory-mediated diseases, including MPNs.
Aims: We investigated if increased NLR is associated with higher all-cause mortality in both the general population and in patients with myeloproliferative neoplasms in a Danish Cohort with 18 years of follow-up.
Methods: Blood cell count measurements were used from The Copenhagen Primary Care Laboratory Database (CopLab), and three hospital-derived Laboratory Information Management Systems from Roskilde, Copenhagen, and the Northern part of Jutland. First, occurring neutrophil and lymphocyte counts were used. Inclusion criteria were an age ≥20 years, hsCRP or CRP <10mg/L. Individuals with inpatient stay or emergency room admissions ±15 days from the sample date were excluded using the Danish National Patient Registry (DNPR), thus allowing only outpatient hospital and general practitioner visits. On included individuals (N=272,933), comorbidities were retrospectively assessed across 19 major disease categories to calculate the Charlson Comorbidity Index score (CCI) using ICD8 and ICD10 codes from DNPR. The sample date for blood count measurements was used as the index date for CCI calculation. MPNs were defined by ICD8 (ET: 28729, PV: 20899, MF: 20900) and ICD10 (ET: DD474 / DD752, PV: DD459, MF: DD474 ). MPN diagnosis after sample date and during follow-up was termed pre-MPN. The CCI score was defined as having 0, 1-2, or >2 comorbidities. NLR was calculated and categorized as NLR <1.5, NLR ≥1.5 - 2, NLR ≥2 - 3, NLR ≥3 - 4, and NLR ≥4. All-cause mortality was ascertained from the National Danish Causes of Death Registry. We used proportional hazard Cox-regression analysis to estimate the hazard ratio (HR) with a 95% confidence interval (95%CI) to investigate all-cause mortality in the general population, MPN patients, and the impact of CCI-score. The analyses were adjusted for age, gender, population, CCI, or NLR.
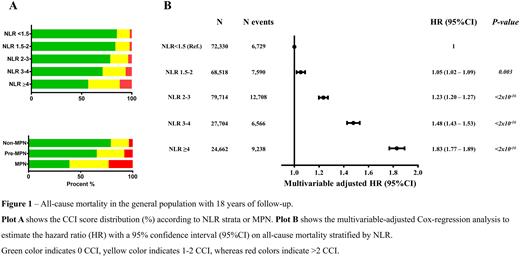
Results: Among 272,933 individuals, 85 had MPN prior to the sample date, whereas 469 developed MPNs during the observation time. Compared to non-MPNs, preMPNs and MPNs had more accumulated comorbidities in both the 1-2 CCI score (17.4% vs. 26.4% vs. 37.7%) and >2 CCI score (4.1% vs. 8.5% vs. 23.5%),P < 2.2x10-16, see figure 1A. For the NLR strata, a stepwise increase in CCI scores was also evident in the 1-2 and >2 CCI scores, P < 2.2x10-16, see figure 1A.
During follow-up with 42,831 events, a stepwise increase in all-cause mortality was observed across the population (see figure 1B). Compared to NLR <1.5 (reference group), NLR 1.5-2 had a HR(95%CI) of 1.05 (1.02 - 1.09), P=0.003, NLR 2-3 had a HR(95%CI) of 1.23 (1.20 - 1.27), P <2x10-16, NLR 3-4 had a HR(95%CI) of 1.48 (1.43- 1.53), P<2x10-16 whereas the highest HR(95%CI) was observed among individuals with NLR ≥4 of 1.83 (1.77-1.89),P <2x10-16.
We also investigated the impact of CCI and MPNs on all-cause mortality. Compared to No MPNs & No CCI (reference group), No MPN with 1-2 or >2 CCI had an HR(95%CI) of 1.90 (1.85 - 1.93), P <2x10-16 and 3.25 (3.16 - 3.35), P<2x10-16, respectively. In contrast, individuals with MPNs & 0 CCI, 1-2 CCI or >2 CCI had a HR(95%CI) of 2.20 (1.39 - 3.50), P=0.0008, 3.62 (2.25 - 2.58), P=1.17x10-7, and 8.15 (4.90 - 13.52), P=4.78x10-16, respectively.
We observed similar results of NLR and MPNs on all-cause mortality.
Conclusion: In a general population study, we observed a stepwise increase in mortality among individuals with higher NLR compared to NLR<1.5. Individuals with higher NLR, preMPN, and MPNs had more comorbidities than those with lower NLR and No MPNs measured by the CCI score.
Disclosures
Hasselbalch:AOP Orphan Pharmaceuticals: Consultancy, Other: Data monitoring board; Novartis: Consultancy, Other: Grants.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal